The year 2020-21 has been a global catastrophe. In England alone, more than 127,000 people have died of Coronavirus, with many tens of thousands still suffering from long Covid.
The epidemic has shown the vulnerability of the oldest among us (mortality is highest amongst older people). It has highlighted the weakness in the way we treat our elderly, who deserve to live their years with dignity and happiness. Unfortunately for the hundreds of thousands of people in care homes, 2020-21 has been a year of isolation, loneliness, and vulnerability.
It doesn’t have to be like this.
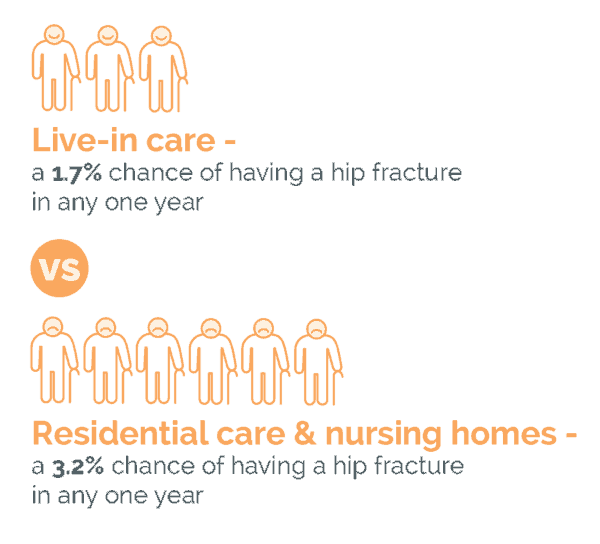
The last year has shown that, even if you need full-time care, you can stay in your own home, have a great quality of life, and see friends and relatives when you choose – while still being safe. A growing body of evidence shows that having a live-in carer gives a far better quality of life for the person who needs care. Live-in care is also within financial reach of almost anybody who owns their own home.
Looking forward: fix the system
The pandemic over the past year and this analysis lay bare the failings in the UKs current institutionalised approach to care. This analysis, commissioned by the Live in Care Hub, uses published data as well as proprietary research by the world renowned Personal Social Services Research Unit (PSSRU), a collaboration between University of Kent and the LSE. The analysis clearly demonstrates that not only do individuals want to remain in their own home should they need care, but it is also safer for them to do so.