The Office for National Statistics has predicted a 36%growth in over 85s between 2015 and 2025, from 1.5 to 2 million across the UK, many of whom will have significant health problems. There’s no doubt this will lead to a substantial increase in demand for care.
As CEO of United Kingdom Homecare Association (UKHCA), my passion is to promote high quality, sustainable care services so people know they can continue to live at home among their local community. It is universally accepted that staying at home is, for the vast majority of people, the preferred option; promoting independence, avoiding or reducing hospital admissions and keeping people in the place they know and love best and among their friends. Our ageing population means that it’s likely we, or our loved ones, will require care at some point. If you’re facing the emotional decision of choosing care, or are an interested healthcare professional, you’ll be keen to discover:
- Where to find the best possible care
- How much it will cost and how to achieve the best value for money
- Whether you, or your family member or patient can stay at home, with pets, in familiar surroundings with friends or family close by
As a unique coalition of leading live-in care providers, The Live-in Care Hub is doing great work to raise awareness of this special, but still little-known service. Over the last four years it has published informative reports with original research, crucial advice and moving stories.
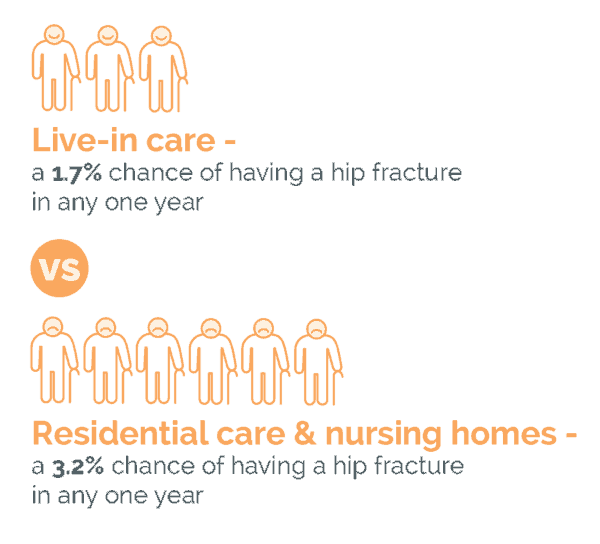
This, the latest report, draws on a wide variety of sources: academic research, Government reports and personal experiences. The findings may be surprising; showing that live-in care ensures a happier and healthier later life – with fewer falls – and is an excellent, affordable alternative to residential or nursing care.
This year’s research, commissioned by The Hub was undertaken by the PSSRU (Personal Social Services Research Unit), a joint venture between the University of Kent and the LSE.