There are now 11.6 million people aged 65* or over in the UK. When it comes to caring for our ageing population, there’s overwhelming evidence that constant, person-centred, one-to-one care produces a far better experience as well as improved health and wellbeing ‘outcomes’ for the vast majority of people. We know that 97 per cent** of people don’t want to go into a residential care home if they become ill or less able to cope; it can be unsettling to move away from friends, a partner or pets. Ageing in our own home – in a safe and therapeutic environment – is the oldest and most respected form of social care, though still little known about in the UK.
So, what is the alternative and how do we know if it’s better?
The Live-in Care Hub is a coalition of leading 24/7 live-in care providers that champion live-in care as a wonderful alternative to residential care. Live-in care means dedicated carers provide around the clock care for people in their own home. Last year it published the No Place Like Home report which looked at our fears for our older loved ones and how we plan (or don’t) for their care.
This year, The Live-in Care Hub’s Better at Home report shares findings from fresh research it has commissioned. It investigates, for the first time, how wellbeing outcomes for people receiving live-in care differ from those in residential or nursing homes.
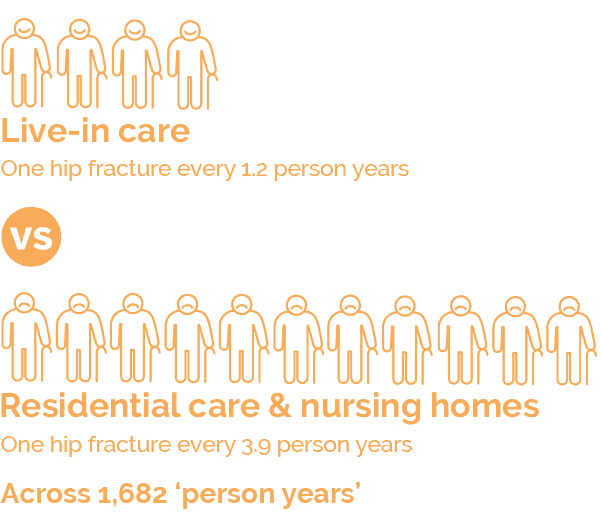
The research, which was conducted by members of The Live-in Care Hub – and their clients, looked at two key areas: falls and associated hip fractures, both of which are major concerns in the health of older people and cost the NHS millions of pounds in hospital admissions.
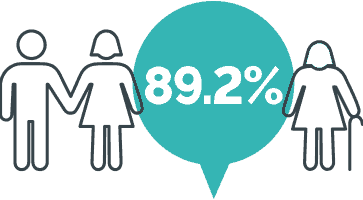
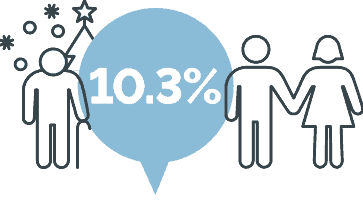
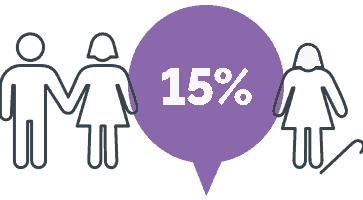
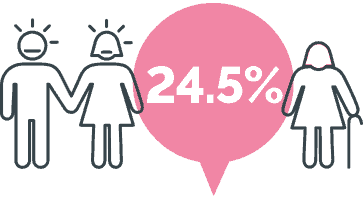
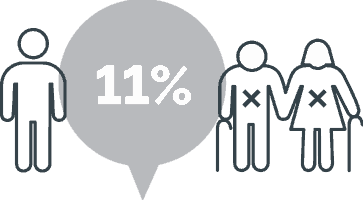
The findings conclusively show that people who have live-in care are less likely to fall, and far less likely to have a hip fracture than people in residential and nursing homes.